Impaired blood flow and stagnation of blood in the venous bed leads to pathological changes in the blood vessels - varicose veins. The reasons for the development of the disease can be different, including genetic predisposition (most often), obesity, hormonal imbalance, pregnancy, arterial hypertension, constipation, lifestyle and professional activity (for example, work that requires long periods of standing inleg. ).
In all these cases, the development of the disease follows the same scenario and is associated with two factors: weakness of the vascular wall and functional insufficiency of the venous valves.
Vascular valves prevent backflow of blood. If they fail to cope with their task, the blood stagnates and collects (deposits) in the veins. As a result, the vessels not only dilate, but also lengthen, become twisted and become intertwined in varicose veins.
Most often, this disease affects the superficial veins (large and small) of the lower extremities. They ensure the outflow of venous blood from the subcutaneous tissue and the skin, which together make up no more than 1/10 of the total circulatory system. The main work is carried out by the deep veins, connected to the superficial veins through perforating venous channels.
The treatment of varicose veins always means the removal or resorption of the vein, i. e. its exclusion from the general venous circulation system. But since such ships play a small role in it, their elimination does not have any negative consequences. Their function is easily taken over by the remaining veins.

Symptoms and stages of the disease
Varicose veins are one of the most common vascular diseases. According to statistics, 10-20% of men and 30-40% of women suffer from it.
The first signs of pathology are the appearance of a blue or red vascular pattern on the skin. This can be a capillary network or stars (telangiectasia). Most often they appear on the legs and thighs, but they can also be found on the face, lips (in women), legs and hands. Spider veins on the face are called rosacea.
Symptoms of varicose veins depend on the stage of the disease. At first it is only heaviness, increased leg fatigue, moderate swelling in the evening, which goes away after rest and sleep. Leg cramps at night are possible.
A characteristic symptom of the disease is pain. Pain in the leg can appear or intensify when walking, standing for a long time or be constant, accompanied by a feeling of saturation, burning and warmth. Enlarged veins become painful when pressed.
In international phlebology, the classification of the disease is from class 0 to class 6.
In the zero phase, there are no visible symptoms; the only complaint may be heaviness in the legs.
In stage 1, a vascular pattern (telangiectasia) appears and muscle cramps occur at night.
Grade 2 disease is manifested by dilated and thick veins that bulge under the skin.
In stage 3, the swelling of the legs (ankles, feet, legs) no longer goes away after a night's sleep, long rest and becomes constant.
In stage 4, the skin over the dilated veins becomes red or blue, areas of hyperpigmentation, itchy skin, dryness, peeling and inflammation appear.
Further, in stages 5 and 6, the development of pre-ulcers and trophic ulcers of the skin follows.
Thus, varicose veins, which begin as an aesthetic problem, can lead to serious health problems over time.
Complications
Stagnation of venous blood and its accumulation (deposit) in the vessels of the lower extremities causes a decrease in blood pressure, hypotension and associated dizziness, fainting and headache.
The skin over the affected vessels becomes thinner, inflamed, develops peeling, itching, congestive dermatitis and varicose eczema, followed by the formation of trophic ulcers.
Blood clots occur in vessels filled with stagnant venous blood, which can break off at any time and, traveling through the general circulatory system, block a vital artery and lead to death.
In the later stages of varicose veins, complications such as phlebitis and thrombophlebitis develop.
The later the treatment of the disease is started, the higher the risk of its complications and the more radical will have to be used to prevent them. Therefore, when the symptoms of varicose veins appear, you should not rely on self-medication, they can be good for prevention. But only a doctor can give real help.

Diagnosis and treatment
As usual, a visit to a doctor begins with a study of complaints, collection of anamnesis and an external examination. The main method for diagnosing varicose veins is Doppler ultrasound, duplex or triplex ultrasound scanning of blood vessels.
As a rule, this method provides a comprehensive picture of the disease to determine the most appropriate treatment tactics.
If additional data is needed, to clarify the diagnosis, the doctor can prescribe a contrast X-ray (radiocontrast venography), MRI of the blood vessels (magnetic resonance venography) or multispiral computed angiography.
Before performing minimally invasive and extensive surgical interventions, a standard set of examinations is prescribed - a general urine test, general clinical and biochemical blood tests, a coagulability test (coagulogram), tests for HIV, syphilis, viral hepatitis, fluorography, ECG. .
In most cases, the treatment of varicose veins in a modern clinic is carried out on an outpatient basis or in a day hospital. It does not require a break from everyday life and after only 1-2 hours you can return to your normal activities. Minimally invasive procedures are performed with or without local anesthesia.
And only radical surgical intervention (phlebectomy) may require short-term hospitalization in the hospital unit of the clinic.
Drug treatment
At an early stage of the development of the disease or for its prevention, the doctor can prescribe drug therapy, including antibiotics and antiseptics (in the presence of inflammation), phleboprotectors, anticoagulants (to prevent thrombosis), phleboprotectors, heparin ointment andother heparins. - containing drugs.
Hirudotherapy can be used as an alternative method of treatment.
Conservative therapy includes wearing compression stockings (thongs, knee socks) and elastic bandages. It has a limited scope.
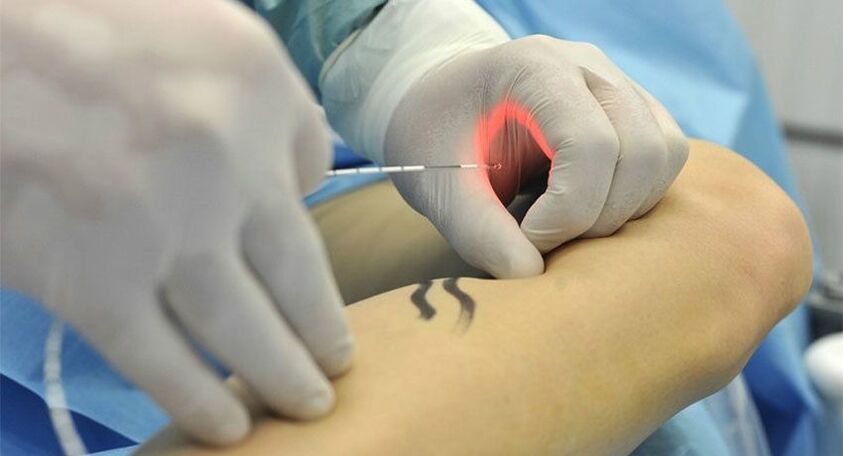
Endovascular laser vascular coagulation (EVLC)
This method refers to minimally invasive methods of treating varicose veins. The procedure is performed under local anesthesia on an outpatient basis. Under ultrasound control, a flexible fiber optic light guide connected to an emitter is inserted into the vascular bed.
Laser light of a certain wavelength is absorbed by blood cells and vein walls and converted into heat.
As a result, the vessel closes and turns into a thin bundle of connective tissue that dissolves on its own.
Laser coagulation is commonly used to treat small and medium-sized varicose veins, especially on the face. But with its help you can also eliminate large varicose veins, including the small and large saphenous veins of the legs.
Radiofrequency ablation
This method, like EVLC, is based on thermal coagulation, only radiofrequency radiation, instead of a laser, is used to seal the container. Otherwise, the procedure is similar. Under local anesthesia, a radio wave emitter is inserted into the venous bed, which is absorbed by the blood and vascular walls, turns into heat and gives a coagulation effect. The procedure is performed under ultrasound guidance.
Like laser coagulation, radiofrequency ablation can be used as the main, single and sufficient method or as part of complex treatment as an additional method. For example, after surgical removal of the main trunk to eliminate smaller vascular branches.
Sclerotherapy
In this case, the varicose vein is sclerosed—glued together from the inside with the help of a sclerosant. This medication is given into a vein through an injection. It can be liquid or foamy.
The procedure is completely painless, during it a slight burning and tingling sensation is possible. To eliminate these sensations, as well as to further compress the vessel, a stream of cold air can be used. This is called cryosclerotherapy.
The use of foam sclerosants has a number of advantages. They have better contact with the vascular wall, which increases the effectiveness of the procedure. To achieve the result, a significantly smaller amount of the sclerosing agent is required, since it is not distributed in the blood.
In addition, it does not spread beyond the area of the procedure, making it easier to control its volume.
Liquid sclerosants are usually used to eliminate small varicose veins, while foam preparations make it possible to sclerose even large veins.
Sclerosis of small veins and capillaries is usually performed under visual control, and the introduction of foam sclerosant into large vessels is performed under ultrasound control.

Miniphlebectomy
This is a minimally invasive surgical method for removing varicose veins. It does not require an incision, anesthesia or epidural.
Treatment for this surgery is performed in a day hospital setting. The doctor performs an ultrasound scan of the vessel and marks it with a marker on the skin. After that, he makes an incision (incision no more than 1-2 mm), through which he takes out part of the vein with a special stroke. This area is clamped and cut.
Next, the doctor moves to the next area, makes an incision, takes out a part of the vein and cuts it. In this way he removes the entire affected ship.
Skin punctures heal quickly and leave no traces, thus achieving an ideal cosmetic effect. The lack of incisions makes the rehabilitation period minimal. Cut vessels are not sewn, and punctures do not require stitching - they are simply closed with an adhesive plaster.
Phlebectomy
This is a classic surgical operation, which has been used less and less recently. It consists in the radical removal of a varicose vein along its entire length. To do this, an incision is made in the groin or under the knee, through which a probe is inserted into the vessel.
With the help of a probe, the vessel is separated from the surrounding tissue and taken out. The operation is performed under general anesthesia or epidural anesthesia.
reHabiLitatiON
After treatment of varicose veins, compression stockings are required. The first days it should be worn around the clock, in the following weeks only during the day and can be removed at night. General restrictions for the rehabilitation period include the exclusion of hot baths, steam baths and saunas.
After minimally invasive operations (laser coagulation, radiofrequency ablation, sclerotherapy, miniphlebectomy), it is recommended to get up and walk around. In the future, walking is recommended as a mandatory part of the rehabilitation course (at least 1 hour per day), while all other physical activities should be limited.
The duration of the rehabilitation period depends on the volume of treatment and surgical intervention.

















